WHAT IS THE HIV CARE CONTINUUM?
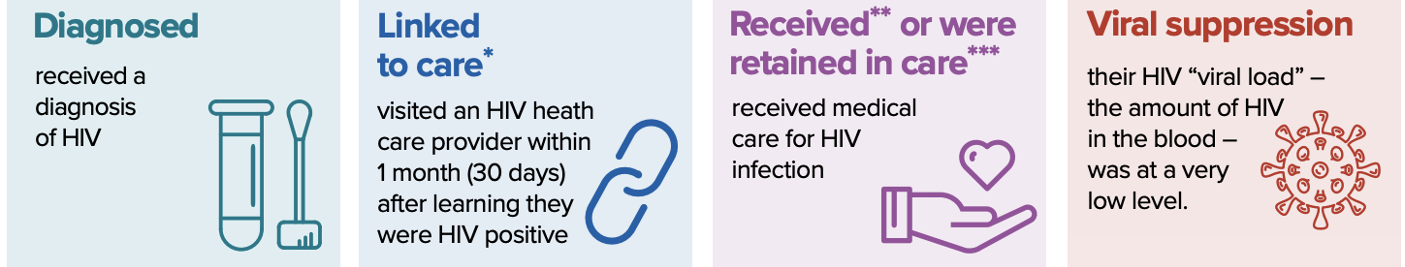
The HIV care continuum is a public health model that outlines the steps or stages that people with HIV go through from diagnosis to achieving and maintaining viral suppression (a very low or undetectable amount of HIV in the body).
The steps are:
-
- Diagnosis of HIV infection
- Linkage to HIV medical care
- Receipt of HIV medical care
- Retention in HIV medical care
- Achievement and maintenance of viral suppression
WHAT ARE THE IAPAC GUIDELINES?
The International Association of Providers of AIDS Care (IAPAC), through a multidisciplinary panel of international advisors, developed the first comprehensive, evidence-based guidelines for optimizing the HIV care continuum, with an aim to increase HIV testing coverage, linkage to care, treatment coverage, engagement and retention in care, and viral suppression for adults and adolescents.
The panel reviewed the scientific literature on the HIV care continuum and made 36 recommendations in six subject areas:
-
- Optimizing the HIV care environment
- Increasing HIV testing coverage and linkage to care
- Increasing HIV treatment coverage
- Increasing retention in care, ART adherence, and viral suppression
- Adolescents
- Metrics for and monitoring of the HIV care continuum
RECOMMENDATIONS FOR OPTIMIZING THE HIV CARE ENVIRONMENT
-
- Laws that criminalize the conduct of or exert punitive legal measures against men who have sex with men (MSM), transgender individuals, people who inject drugs (PWID), and sex workers are not recommended and should be repealed where they have been enacted. (A IV)
- Laws that criminalize the conduct of people with HIV based on perceived exposure to HIV, and without any evidence of intent to do harm, are not recommended and should be repealed where they have been enacted. (A IV)
- HIV-related restrictions on entry, stay, and residence in any country for people with HIV are not recommended and should be repealed where they have been enacted. (A IV)
- Strategies to monitor for and eliminate stigma and discrimination based on race, ethnicity, gender, age, sexual orientation, and/or behavior in all settings, but particularly in healthcare settings, using standardized measures and evidence-based approaches, are recommended. (B II)
- Proactive steps are recommended to identify and manage clinical mental health disorders (e.g., anxiety, depression, and traumatic stress) and/or mental health issues related to HIV diagnosis, disclosure of HIV status, and/or HIV treatment. (A II)
- Enabling people with HIV to take responsibility for their care (e.g., self-management, user-driven care) is recommended. (B I)
- Shifting and sharing HIV testing, dispensing of antiretroviral therapy (ART), and other appropriate tasks among professional and paraprofessional health worker cadres is recommended. (A I)
-
- Use of lay health workers to provide pretest education and testing and to enhance engagement of people with HIV in medical care is recommended. (B I)
- Task shifting/sharing from physicians to appropriately trained healthcare providers, including nurses and associate clinicians, is recommended for ART initiation and maintenance. (B II)
-
- Community engagement in every step across the HIV care continuum is recommended. (B II)
RECOMMENDATIONS FOR INCREASING HIV TESTING COVERAGE AND LINKAGE TO CARE
-
- Routinely offering opt-out HIV testing to all individuals who present at health facilities is recommended. (A I)
- Community-based HIV testing is recommended to reach those who are less likely to attend facility-based HIV testing. (A I)
- Confidential, voluntary HIV testing in large workplace and institutional settings (military, police, mining/trucking companies, and educational venues) should be considered. (B III)
- HIV self-testing is recommended with the provision of guidance about the proper method for administering the test and direction on what to do once the results have been obtained. (B II)
- Use of epidemiological data and network analyses to identify individuals at risk of HIV infection for HIV testing is recommended. (B II)
- The offer of HIV testing to partners of newly diagnosed individuals is recommended. (A I)
- Immediate referral to HIV care is recommended following an HIV-positive diagnosis to improve linkage to ART. (A I)
- For high-risk individuals who test HIV-negative, offering pre-exposure prophylaxis (PrEP) is recommended in addition to the provision of free condoms, education about risk reduction strategies, post-exposure prophylaxis (PEP), and voluntary medical male circumcision. (A I)
- Use of case managers and patient navigators to increase linkage to care is recommended. (B II)
RECOMMENDATIONS FOR INCREASING HIV TREATMENT COVERAGE
-
- The immediate offer of ART after HIV diagnosis, irrespective of CD4 cell count or clinical stage, is recommended. (A I)
- First-line ART regimens with the highest levels of efficacy, lowest adverse event profiles, and delivered in once-daily fixed-dose combinations are recommended. (B II)
- Viral load testing at least every 6 months is recommended as the preferred tool for monitoring ART response. (B II)
- HIV drug resistance testing is recommended at entry into care or prior to ART initiation and when virologic failure is confirmed. (BI)
-
- Where routine access to HIV drug resistance testing is restricted, population-based surveillance is recommended. (BII)
-
- Community-located ART distribution is recommended. (A II)
-
- The use of community-based pharmacies should be considered. (C III)
-
RECOMMENDATIONS FOR INCREASING RETENTION IN CARE, ART ADHERENCE, AND VIRAL SUPPRESSION
-
- Systematic monitoring of retention in HIV care is recommended for all patients. (A II)
-
- Retention in HIV care should be considered as a quality indicator. (B III)
- Measuring HIV care retention using electronic health record and other health system data is recommended. (BII)
- Use of clinic databases/surveillance systems for HIV clinical monitoring and population-level tracking is recommended. (B II)
-
- Routine ART adherence monitoring is recommended in all patients. (A II)
-
- Viral suppression is recommended as the primary adherence monitoring metric. (B II)
- Routine collection of self-reported patient adherence data is recommended. (A II)
- Pharmacy refill data are recommended for adherence monitoring. (B II)
-
- Information and communication technologies aimed at supporting patient self-care are recommended. (B II)
-
- Mobile health technology using weekly interactive components (e.g., 2-way text messaging) is recommended. (B I)
- Alarm devices are recommended as reminders for people with HIV with memory impairment. (A I)
-
- Patient education about and offering support for medication adherence and keeping clinic appointments are recommended. (A I)
-
- Pillbox organizers are recommended, particularly for people with HIV with lifestyle-related barriers to adherence. (B II)
-
- Neither directly administered nor directly observed ART is recommended for routine clinical care settings. (A I)
-
- Directly administered ART is recommended for PWID and previously incarcerated individuals at high risk of ART non-adherence. (B I)
-
- Proactive engagement and reengagement of patients who miss clinic appointments and/or are lost to follow-up, including intensive outreach for those not engaged in care within one month of a new HIV diagnosis, is recommended. (B II)
-
- Case management to retain people with HIV in care and locate and reengage patients lost to follow-up is recommended. (B II)
- Transportation support for people with HIV to attend their clinic visits is recommended. (B II)
-
- Systematic monitoring of retention in HIV care is recommended for all patients. (A II)
RECOMMENDATIONS FOR ADOLESCENTS AND THE HIV CARE CONTINUUM
-
- Removing adult-assisted consent to HIV testing and counseling is recommended for minor adolescents with the capacity to consent. (B II)
- Adolescent-centered services are recommended in both clinical and community-based settings. (A IV)
- Informing an adolescent of their HIV-positive diagnosis is recommended as soon after diagnosis as feasible. (B II)
- A transition plan between pediatric and adult HIV care is recommended. (B II)
RECOMMENDATIONS FOR METRICS FOR AND MONITORING OF THE HIV CARE CONTINUUM
-
- A standardized method should be used to estimate the total number of people with HIV (diagnosed and undiagnosed) within a geographic setting. (A IV)
- The estimated number of people with HIV in the geographic setting should be the overall denominator for the HIV care continuum. (A IV)
- Collection of a minimum set of 5 data elements should be considered to populate the HIV care continuum. (A IV)
-
- Estimated number of people with HIV
- Number and proportion of people with HIV who are diagnosed as having HIV
- Number and proportion of people with HIV who are linked to care (optional)
- Number and proportion of people with HIV on ART
- Number and proportion of people with HIV on ART who are virally suppressed
-
- Where possible, jurisdictions should consider longitudinal cohort measurement of HIV service utilization and treatment outcomes to identify the means to maximize viral suppression through ensuring early access to ART and retention in care. (A IV)
WHAT’S THE BOTTOM LINE?
The IAPAC guidelines are the first evidence-based recommendations to improve the care environment for people with HIV.
MORE INFORMATION
Full text of the IAPAC guidelines
Reviewed June 2024
Print PDF




