WHAT IS THE HIV CARE CONTINUUM?
The HIV care continuum is a public health model that outlines the steps or stages that people with HIV go through from diagnosis to achieving and maintaining viral suppression (a very low or undetectable amount of HIV in the body). Specifically, the Centers for Disease Control and Prevention (CDC) tracks:
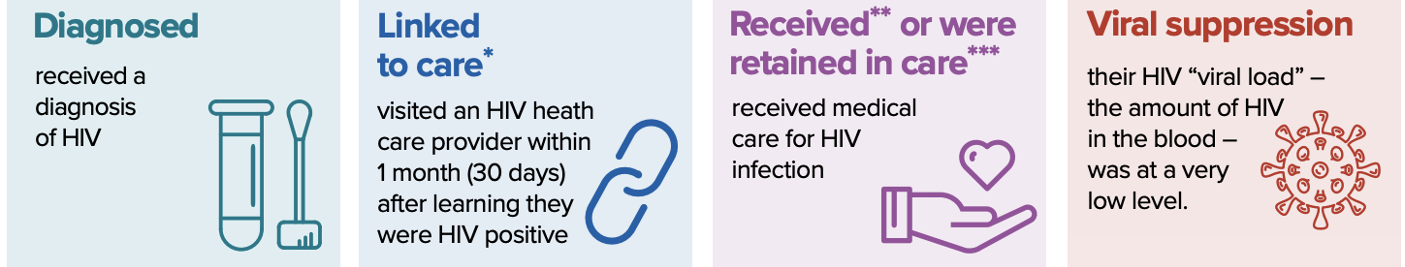
The steps are:
-
- Diagnosis of HIV infection (HIV testing)
- Getting into medical care
- Staying in medical care
- Achieving viral suppression (undetectable viral load)
Antiretroviral therapy (ART) can reduce the risk of serious illness, death, or transmission of HIV. ART is recommended for all people with HIV in a strategy called treatment as prevention (TasP). Yet, only half of people with HIV around the world are aware of their status. Among those who know their HIV status, many do not receive ART in a timely manner, fail to stay engaged in care, or do not achieve sustained viral suppression.
WHY IS THE HIV CARE CONTINUUM IMPORTANT?
The HIV care continuum is useful both as an individual-level tool to assess care outcomes, as well as a population-level framework to analyze the proportion of people with HIV in a given community who are engaged in each successive step. The care continuum can help communities and health programs prevent new infections, improve health, and understand how people with HIV receive care and treatment.
Supporting people with HIV to move through the steps of the continuum to achieve and maintain viral suppression is critical. There are important health benefits to getting the viral load as low as possible: people with HIV who get and keep an undetectable viral load can live long, healthy lives. There is also a major prevention benefit: people with HIV who take HIV medicine daily as prescribed and get and keep an undetectable viral load have effectively no risk of transmitting HIV to their HIV-negative sexual partners (Undetectable = Untransmittable or U=U).
For people with HIV to receive these benefits, they need to know that they have HIV, receive medical care, and stay on treatment with antiretroviral medications (ARVs). However, there are obstacles to getting HIV care and treatment, substantially limiting the effectiveness of efforts to improve health outcomes for people with HIV and reduce new HIV transmissions.
Knowing where the gaps are most pronounced, and for what populations, is vital to knowing how, where, and when to intervene to break the cycle of HIV transmission.
HOW IS THE HIV CARE CONTINUUM BEING USED?
Federal, state, and local health departments, community-based organizations, healthcare providers, and people with HIV continue to use the HIV care continuum to measure progress toward HIV goals as well as to pinpoint where gaps in services may exist in connecting people with HIV to sustained, quality care and treatment. Knowing where drop-offs are most pronounced, and for what populations, helps policymakers and healthcare providers implement system improvements to support all people with HIV who are able to successfully navigate the continuum and achieve viral suppression.
WHAT’S THE BOTTOM LINE?
The HIV care continuum describes how people with HIV get diagnosed, engage in medical care, receive ART, and achieve undetectable HIV viral loads. Monitoring the HIV care continuum is critical to ensure that all people with HIV benefit from care and treatment.
MORE INFORMATION
HIV.gov: HIV Care Continuum
CDC: Understanding the HIV Care Continuum
Reviewed June 2024
Print PDF




